Cataplexy is a sudden and temporary loss of muscle control that can occur in people with narcolepsy.
Cataplexy is a rare condition that affects approximately 70% of people with narcolepsy. Cataplexy can be triggered by strong emotions such as laughter, excitement, or anger, and can cause a person to collapse or fall down.
During a cataplexy episode, the person remains fully conscious but is unable to move or speak. The episode usually lasts for a few seconds to a few minutes, and the person may experience weakness in their limbs, slurred speech, or drooping eyelids. Although cataplexy is not dangerous, it can be embarrassing or disruptive to daily life, and may cause anxiety or depression in some people.
The exact cause of cataplexy is not fully understood, but it is thought to be related to a deficiency of a neurotransmitter called hypocretin. Treatment for cataplexy typically involves medications that help to regulate the levels of hypocretin in the brain, as well as lifestyle changes such as avoiding triggers that can cause episodes. With proper management, most people with cataplexy can lead normal and fulfilling lives.
Understanding Cataplexy
Definition and Symptoms
Cataplexy is a sudden and temporary loss of muscle tone, which can cause partial or complete muscle weakness, collapse, or paralysis. It is a symptom of narcolepsy, a sleep disorder that causes excessive daytime sleepiness. Cataplexy can be triggered by strong emotions such as laughter, anger, or surprise. Symptoms of cataplexy can vary from person to person, and can range from mild to severe.
Causes and Pathophysiology
Cataplexy is caused by a loss of orexin (also known as hypocretin), a neurotransmitter that regulates wakefulness and sleep. Orexin is produced by brain cells in the hypothalamus. In people with narcolepsy, these brain cells are damaged or destroyed, resulting in a loss of orexin. This loss of orexin can cause a range of symptoms, including cataplexy and excessive daytime sleepiness.
Relation to Narcolepsy
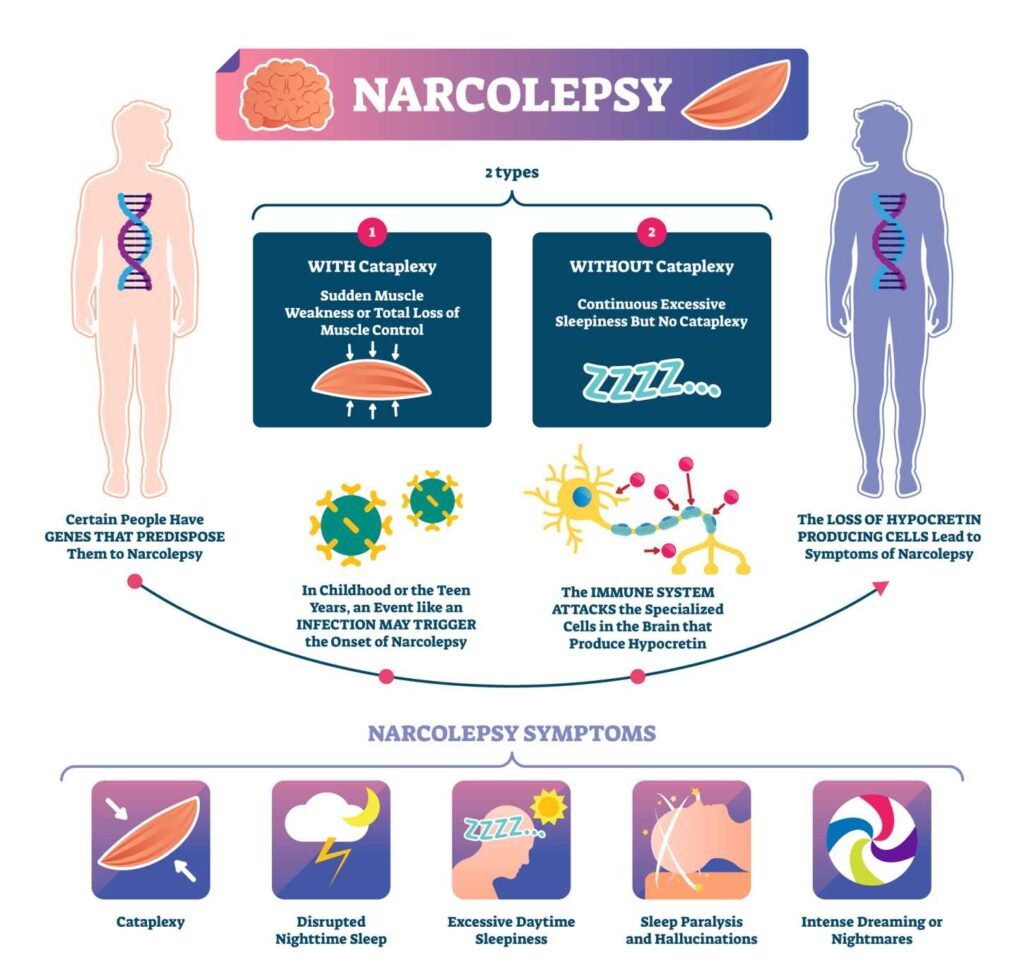
Cataplexy is a hallmark symptom of narcolepsy, a sleep disorder that affects approximately 1 in 2,000 people. There are two types of narcolepsy: type 1 and type 2.
Type 1 narcolepsy is characterized by excessive daytime sleepiness, cataplexy, and other symptoms such as sleep paralysis and hallucinations.
Type 2 narcolepsy is characterized by excessive daytime sleepiness and other symptoms, but does not typically include cataplexy.
Overall, cataplexy is a complex symptom that is closely related to narcolepsy. While the exact causes of cataplexy are not fully understood, it is believed to be caused by a loss of orexin in the brain. Understanding the underlying causes and mechanisms of cataplexy is important for developing effective treatments for this symptom and for improving the quality of life of people with narcolepsy.
Identifying Cataplexy
Cataplexy is a sudden loss of muscle tone triggered by strong emotions such as laughter, anger, or stress. It is a hallmark symptom of narcolepsy, a neurological disorder that affects the sleep-wake cycle. Identifying cataplexy can be challenging, as it can be mistaken for other conditions that cause muscle weakness or paralysis.
Common Triggers
Emotional triggers are the most common cause of cataplexy. People with cataplexy may experience sudden episodes of muscle weakness or paralysis when they are laughing, excited, angry, or stressed. The severity of cataplexy can vary from mild weakness in the facial muscles to complete collapse of the body.
Diagnosis Process
Diagnosing cataplexy requires a thorough evaluation by a healthcare provider. The diagnosis is typically based on a combination of clinical symptoms, medical history, and diagnostic tests. The most common test used to diagnose cataplexy is the Multiple Sleep Latency Test (MSLT), which measures the time it takes for a person to fall asleep during the day.
In addition to the MSLT, a healthcare provider may also perform a cerebrospinal fluid analysis to detect low levels of hypocretin, a neurotransmitter that regulates wakefulness. Other diagnostic tests may include an electroencephalogram (EEG) or a polysomnogram (PSG) to evaluate sleep patterns and detect any underlying sleep disorders.
Overall, identifying cataplexy requires a comprehensive evaluation by a healthcare provider. If you or someone you know is experiencing sudden episodes of muscle weakness or paralysis, it is important to seek medical attention to determine the underlying cause and receive appropriate treatment.
Living with Cataplexy
Cataplexy is a chronic condition that can significantly impact a person’s daily life. However, with proper management and support, individuals with cataplexy can lead a fulfilling life. This section will discuss the daily management and coping strategies that can help individuals with cataplexy manage their condition.
Daily Management
Managing cataplexy requires a combination of lifestyle changes and medication. Lifestyle changes such as maintaining a regular sleep schedule, avoiding alcohol and caffeine, and reducing stress can help reduce the frequency and severity of cataplexy attacks. Medications such as antidepressants and sodium oxybate can also be used to manage cataplexy.
Support and Coping Strategies
Living with cataplexy can be challenging, and individuals with cataplexy may benefit from support and coping strategies. It is important to have a care team that includes a physician, a sleep specialist, and a mental health professional. A support group can also provide individuals with cataplexy with a sense of community and understanding.
Coping strategies such as mindfulness meditation, deep breathing exercises, and progressive muscle relaxation can help individuals with cataplexy manage stress and reduce the frequency of cataplexy attacks. Regular exercise, such as yoga or swimming, can also help improve quality of life and reduce stress.
In conclusion, living with cataplexy can be challenging, but with proper management and support, individuals with cataplexy can lead a fulfilling life. Daily management and coping strategies such as lifestyle changes, medication, and support groups can help individuals with cataplexy manage their condition and improve their quality of life.
Treatment Options
Medications
There are several medications available to treat cataplexy. Sodium oxybate is a medication that has been approved by the FDA for the treatment of cataplexy. It is a central nervous system depressant that can reduce the frequency and severity of cataplexy attacks. Antidepressants, such as tricyclic antidepressants and venlafaxine, can also be used to treat cataplexy. These medications can help to regulate the levels of neurotransmitters in the brain, which can reduce the occurrence of cataplexy attacks.
Pitolisant is a medication that has been recently approved by the FDA for the treatment of cataplexy. It is a selective histamine H3 receptor antagonist/inverse agonist that can help to reduce the frequency and severity of cataplexy attacks. Modafinil and stimulants can also be used to treat cataplexy. These medications can help to improve wakefulness and reduce the occurrence of cataplexy attacks.
Non-Pharmacological Interventions
In addition to medications, there are several non-pharmacological interventions that can be used to treat cataplexy. Lifestyle changes, such as improving sleep hygiene and increasing exercise, can help to reduce the frequency and severity of cataplexy attacks. Support from family, friends, and healthcare professionals can also be beneficial for individuals with cataplexy.
Sleep hygiene refers to the practices and habits that can help to promote good sleep. These practices include maintaining a consistent sleep schedule, avoiding caffeine and alcohol before bedtime, and creating a comfortable sleep environment. Exercise can also be beneficial for individuals with cataplexy. Regular exercise can help to improve overall health and reduce stress, which can reduce the occurrence of cataplexy attacks.
Overall, the treatment of cataplexy requires a comprehensive approach that includes both medications and non-pharmacological interventions. With the right treatment plan, individuals with cataplexy can manage their symptoms and improve their quality of life.
Associated Conditions
Comorbid Sleep Issues
Cataplexy is a symptom of narcolepsy, a sleep disorder that affects the normal sleep-wake cycle. People with narcolepsy often experience excessive daytime sleepiness, sudden sleep attacks, sleep paralysis, and hypnagogic hallucinations. These symptoms can significantly affect their quality of life and daily activities.
Sleep paralysis is a condition in which a person is unable to move or speak while falling asleep or waking up. It can be a terrifying experience, especially if accompanied by hallucinations. Sleep paralysis is often associated with narcolepsy and can occur during cataplexy attacks.
Other Related Disorders
Cataplexy can also occur in other conditions, such as Niemann-Pick Type C disease, Prader-Willi syndrome, and Angelman syndrome. These are rare genetic disorders that affect the nervous system and can cause a range of symptoms, including cataplexy.
Autoimmune disorders, such as multiple sclerosis and lupus, can also cause cataplexy-like symptoms. In these conditions, the immune system attacks the body’s own tissues, including the nervous system, leading to a range of neurological symptoms.
It is important to note that not all cases of cataplexy are associated with other conditions. In some cases, cataplexy can occur as an isolated symptom without any underlying medical condition.
Overall, cataplexy can be a debilitating symptom that can significantly affect a person’s quality of life. Understanding the associated conditions can help with early diagnosis and appropriate treatment.
Precautions and Safety
Navigating Daily Activities
Individuals with cataplexy may experience sudden muscle weakness or paralysis, which can result in falls or accidents. Therefore, it is essential to take necessary precautions while performing daily activities such as walking, climbing stairs, or carrying heavy objects. It is recommended to use assistive devices such as canes or walkers to provide support and stability.
Avoiding Aggravating Factors
Certain factors can trigger cataplexy episodes, which can be avoided or minimized to reduce the frequency and severity of attacks. These factors include:
- Driving: Individuals with cataplexy should avoid driving or operating heavy machinery, as sudden muscle weakness can lead to accidents.
- Exercise: Vigorous physical activity can trigger cataplexy episodes, and it is recommended to engage in low-impact exercises such as yoga or swimming.
- Sleep Deprivation: Lack of sleep can worsen cataplexy symptoms, and it is recommended to get adequate sleep to reduce the frequency of attacks.
- Alcohol and Caffeine: These substances can trigger cataplexy episodes and should be avoided or consumed in moderation.
- Stress and Fatigue: Emotional stress and physical fatigue can trigger cataplexy episodes, and it is recommended to manage stress levels and take regular breaks to avoid exhaustion.
By taking necessary precautions and avoiding aggravating factors, individuals with cataplexy can reduce the frequency and severity of attacks and lead a safe and healthy life.
Advancements in Research
Neurological Insights
Recent research has shed light on the neurological mechanisms underlying cataplexy. It has been discovered that cataplexy is caused by a sudden inhibition of motor neurons in the brainstem, leading to muscle weakness and loss of control. This inhibition is triggered by the release of neurotransmitters such as GABA and histamine, which act on receptors in the brain.
Furthermore, studies have found that cataplexy is often associated with brain injury, particularly in the hypothalamus and amygdala regions. This suggests that these areas of the brain may play a crucial role in regulating the body’s response to emotional stimuli, which can trigger cataplexy in individuals with narcolepsy.
Future Therapies
There are currently no cures for cataplexy, but several promising therapies are being developed. One such therapy is Xyrem, a drug that works by increasing the levels of the neurotransmitter GABA in the brain. This has been shown to reduce the frequency and severity of cataplexy attacks in some individuals.
Other potential therapies include medications that target histamine and epinephrine receptors in the brain, as well as non-invasive brain stimulation techniques such as transcranial magnetic stimulation (TMS). These therapies hold great promise for improving the lives of individuals with cataplexy and narcolepsy.
In conclusion, advancements in research have provided valuable insights into the neurological mechanisms underlying cataplexy and have paved the way for the development of new therapies. While there is still much to learn about this condition, these advancements offer hope for a brighter future for those affected by cataplexy.
Frequently Asked Questions
What are the common symptoms of cataplexy?
Cataplexy is a sudden loss of muscle tone that can be triggered by strong emotions such as laughter, anger, or excitement. The most common symptom of cataplexy is a sudden weakness or paralysis of the muscles, which can cause a person to fall to the ground or become unable to move. Other symptoms may include slurred speech, drooping eyelids, and difficulty breathing.
How is cataplexy typically treated?
There is no cure for cataplexy, but there are several treatment options available to manage the symptoms. Medications such as antidepressants and sodium oxybate can help reduce the frequency and severity of cataplexy attacks. Lifestyle changes such as avoiding triggers, getting enough sleep, and practicing relaxation techniques can also be helpful.
What triggers a cataplexy attack?
Cataplexy attacks are often triggered by strong emotions such as laughter, anger, or excitement. Other triggers may include stress, physical exertion, or sudden changes in temperature.
What is the distinction between cataplexy and catalepsy?
Cataplexy and catalepsy are both conditions that involve a loss of muscle tone, but they are caused by different underlying conditions. Cataplexy is a symptom of narcolepsy, while catalepsy is a symptom of certain neurological disorders such as Parkinson’s disease.
How does narcolepsy with cataplexy differ from narcolepsy without it?
Narcolepsy is a sleep disorder that causes excessive daytime sleepiness and other symptoms such as sleep paralysis and hallucinations. Narcolepsy with cataplexy is a subtype of narcolepsy that also includes episodes of cataplexy. Narcolepsy without cataplexy does not involve cataplexy episodes.
Can you provide examples of what might happen during a cataplexy episode?
During a cataplexy episode, a person may experience sudden weakness or paralysis of the muscles. This can cause them to fall to the ground or become unable to move. They may also experience slurred speech, drooping eyelids, and difficulty breathing. The symptoms usually last for a few seconds to a few minutes before resolving on their own.
10-3-2-1-0 Sleep Rule: A Simple Guide to Better Sleep

The 10-3-2-1-0 sleep rule is designed to help individuals maintaining a regular sleep schedule that promotes restful and restorative sleep. By following this rule, individuals can create a relaxing environment that signals to the body that it is time to sleep.
Continue reading about the: 10-3-2-1-0 Sleep Rule
MaryRuth Organics Sleep Gummies Without Melatonin Review: Do They Work?

These gummies are designed to promote relaxation and support sleep quality for adults. Unlike many other sleep aids, they don’t contain melatonin, so you won’t wake up feeling groggy or drowsy.
Continue reading: MaryRuth Organics Sleep Gummies Without Melatonin




