Circadian rhythm sleep-wake disorders are a group of sleep disorders that affect the timing of sleep and wake cycles.
Circadian rhythm sleep-wake disorders are caused by a disruption in the body’s circadian rhythm, which is the internal biological clock that regulates the sleep-wake cycle. The circadian rhythm is influenced by various factors, including light exposure, social and work schedules, and hormonal changes.
There are several types of circadian rhythm sleep-wake disorders, including delayed sleep phase disorder, advanced sleep phase disorder, non-24-hour sleep-wake disorder, irregular sleep-wake rhythm, and shift work disorder. Each type of disorder is characterized by a specific pattern of sleep disturbance and affects individuals differently. Some people may have difficulty falling asleep at night, while others may have trouble staying awake during the day.
Circadian rhythm sleep-wake disorders can have a significant impact on an individual’s quality of life, affecting their ability to function during the day and causing fatigue, irritability, and difficulty concentrating. Treatment options for these disorders include light therapy, behavioral therapy, and medication. It is important for individuals who suspect they may have a circadian rhythm sleep-wake disorder to consult with a healthcare professional for an accurate diagnosis and appropriate treatment.
Understanding Circadian Rhythms
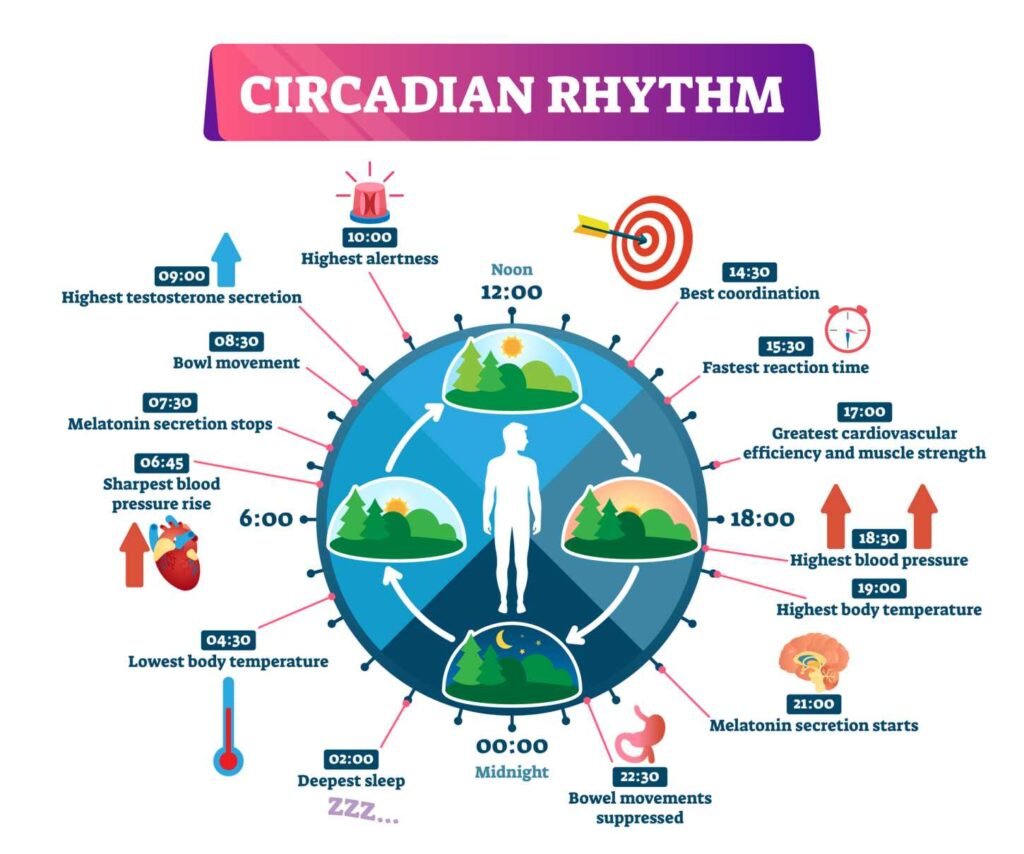
Circadian rhythms are biological processes that follow a 24-hour cycle. These rhythms regulate various physiological functions, including the sleep-wake cycle, hormone secretion, and body temperature. The sleep-wake cycle is one of the most important circadian rhythms, and disruptions to this cycle can lead to circadian rhythm sleep-wake disorders.
Biological Clock and Sleep-Wake Cycle
The biological clock is responsible for regulating the sleep-wake cycle. The sleep-wake cycle is a 24-hour cycle that determines when we sleep and when we wake up. The biological clock is located in the suprachiasmatic nucleus (SCN) of the hypothalamus. The SCN receives information about light and dark cycles from the eyes, which helps to regulate the sleep-wake cycle.
Role of the Suprachiasmatic Nucleus (SCN)
The suprachiasmatic nucleus is responsible for regulating the sleep-wake cycle. It receives information about light and dark cycles from the eyes and uses this information to regulate the release of melatonin, a hormone that helps to regulate sleep. The SCN also regulates other physiological functions, including body temperature and hormone secretion.
Influence of Light on Circadian Rhythms
Light is one of the most important factors that influence circadian rhythms. Exposure to bright light in the morning helps to reset the biological clock and promote wakefulness. Exposure to dim light or blue light in the evening can disrupt the sleep-wake cycle and make it harder to fall asleep. Artificial light can also disrupt the sleep-wake cycle, especially if it is used late at night. Sunlight is the best source of light therapy and can help to regulate the sleep-wake cycle.
In conclusion, understanding circadian rhythms is essential for maintaining a healthy sleep-wake cycle. The biological clock, located in the SCN, is responsible for regulating the sleep-wake cycle. Light is one of the most important factors that influence circadian rhythms, and exposure to bright light in the morning can help to promote wakefulness.
There are affiliate links on this page, which means we may earn a small commission should you buy after clicking on one, or more of those links. At no extra cost to you.
Types of Circadian Rhythm Sleep-Wake Disorders
Circadian rhythm sleep-wake disorders (CRSWDs) are a group of sleep disorders that affect the timing of sleep and wakefulness. There are five main types of CRSWDs, each with its own unique characteristics and symptoms.
Delayed Sleep-Wake Phase Disorder (DSWPD)
Delayed Sleep-Wake Phase Disorder (DSWPD) is a type of CRSWD that is characterized by a delayed sleep-wake cycle. People with DSWPD have difficulty falling asleep at a conventional time and often stay awake until the early hours of the morning. As a result, they tend to wake up later in the day and experience difficulty waking up in the morning.
Advanced Sleep-Wake Phase Disorder (ASWPD)
Advanced Sleep-Wake Phase Disorder (ASWPD) is the opposite of DSWPD. People with ASWPD have an earlier sleep-wake cycle, meaning they tend to fall asleep and wake up earlier than most people. This can cause difficulty staying awake in the evening and waking up too early in the morning.
Irregular Sleep-Wake Rhythm Disorder (ISWRD)
Irregular Sleep-Wake Rhythm Disorder (ISWRD) is a type of CRSWD that is characterized by a lack of a regular sleep-wake cycle. People with ISWRD may experience multiple sleep episodes throughout the day and night, with no clear pattern or regularity. This can lead to difficulty maintaining a consistent sleep schedule.
Non-24-Hour Sleep-Wake Rhythm Disorder (N24SWD)
Non-24-Hour Sleep-Wake Rhythm Disorder (N24SWD) is a type of CRSWD that is most commonly seen in people who are blind. It is characterized by a sleep-wake cycle that is longer than 24 hours, which can cause a person’s sleep-wake schedule to shift later and later each day. This can lead to difficulty falling asleep at a conventional time and waking up at a reasonable hour.
Shift Work Sleep Disorder
Shift work sleep disorder is a type of CRSWD that is caused by working irregular or night-time shifts. People with shift work sleep disorder may experience difficulty falling asleep during the day and staying awake at night. This can lead to sleepiness and fatigue during work hours, which can affect job performance and safety.
Overall, CRSWDs can have a significant impact on a person’s quality of life. It is important to seek medical attention if you suspect you may have a CRSWD, as treatment options are available.
Symptoms and Diagnosis
Common Symptoms of CRSDs
Individuals with Circadian Rhythm Sleep-Wake Disorders (CRSDs) may experience a range of symptoms that affect their sleep quality and daytime functioning. Some of the common symptoms of CRSDs include difficulty falling asleep or staying asleep, daytime sleepiness, fatigue, irritability, and decreased productivity.
Excessive Daytime Sleepiness (EDS) is a hallmark symptom of many CRSDs, and it is often accompanied by poor sleep quality. Individuals with CRSDs may also experience disrupted sleep patterns, such as insomnia, hypersomnia, or irregular sleep-wake cycles.
Diagnostic Criteria and Methods
The clinical diagnosis of CRSDs requires a thorough evaluation of the individual’s sleep history, physical examination, and laboratory tests. The International Classification of Sleep Disorders (ICSD) provides diagnostic criteria and guidelines for the identification and classification of CRSDs.
Diagnostic methods may include sleep diaries, actigraphy monitoring, and polysomnography (PSG). Sleep diaries are useful for tracking sleep-wake patterns and identifying potential triggers for sleep disturbances. Actigraphy monitoring involves the use of a wrist-worn device that records movement and light exposure to estimate sleep-wake cycles. PSG is a comprehensive sleep study that measures various physiological parameters, such as brain waves, muscle activity, and eye movements, to diagnose sleep disorders.
Use of Sleep Diaries and Actigraphy Monitoring
Sleep diaries and actigraphy monitoring are non-invasive, cost-effective, and easy-to-use methods for monitoring sleep-wake patterns in individuals with CRSDs. Sleep diaries can provide valuable information about the timing, duration, and quality of sleep, as well as any associated symptoms or triggers. Actigraphy monitoring can provide objective data on sleep-wake cycles, light exposure, and physical activity, which can be used to identify circadian rhythm disturbances.
In conclusion, the diagnosis of CRSDs requires a comprehensive evaluation of the individual’s sleep history, physical examination, and laboratory tests. Sleep diaries and actigraphy monitoring are useful tools for monitoring sleep-wake patterns and identifying potential triggers for sleep disturbances. The use of diagnostic criteria and methods outlined in the ICSD can help clinicians accurately diagnose CRSDs and develop appropriate treatment plans.
Etiology and Prevalence
Genetic and Environmental Factors
Circadian rhythm sleep-wake disorders (CRSWDs) are caused by a combination of genetic and environmental factors. Genetic factors play a significant role in the etiology of CRSWDs. Studies have shown that certain genes, such as PER1, PER2, PER3, CRY1, and CRY2, are involved in regulating the circadian rhythm. Mutations in these genes can lead to disruptions in the sleep-wake cycle, resulting in various types of CRSWDs.
Environmental factors, such as exposure to light, also play a crucial role in regulating the circadian rhythm. Exposure to bright light in the morning can help reset the circadian clock, while exposure to light at night can disrupt it. Night shift work, frequent travel across time zones, and aging can all lead to disruptions in the circadian rhythm, resulting in CRSWDs.
Influence of Lifestyle and Occupation
Lifestyle factors, such as alcohol and caffeine consumption, can also affect the circadian rhythm. Alcohol can disrupt sleep, while caffeine can interfere with the production of melatonin, a hormone that regulates the sleep-wake cycle. Certain occupations, such as those that require night shift work, can also increase the risk of developing CRSWDs.
Statistics and Commonality
CRSWDs are relatively common, affecting up to 10% of the general population. The prevalence of CRSWDs varies depending on the type of disorder. Delayed sleep phase disorder (DSPD) is the most common type of CRSWD, accounting for approximately 75% of all cases. Advanced sleep phase disorder (ASPD) is less common, accounting for only 1% of cases. Non-24-hour sleep-wake disorder (N24SWD) is rare, affecting less than 1% of the population.
In conclusion, CRSWDs are caused by a complex interplay of genetic and environmental factors. Lifestyle factors and occupation can also contribute to the development of CRSWDs. While CRSWDs are relatively common, they can be effectively managed with appropriate treatment and lifestyle modifications.
Treatment and Management
Chronotherapy and Light Therapy
Chronotherapy and light therapy are two commonly used treatments for circadian rhythm sleep-wake disorders. Chronotherapy involves gradually shifting the sleep-wake cycle by delaying or advancing the sleep schedule by a few hours each day until the desired sleep-wake cycle is achieved. Light therapy involves exposing individuals to bright light in the morning or evening to reset the circadian rhythm.
Pharmacological Therapies
Pharmacological therapies are another option for treating circadian rhythm sleep-wake disorders. Melatonin is a hormone that can be used to help regulate the sleep-wake cycle. Tasimelteon, a melatonin receptor agonist, has also been approved by the FDA for the treatment of non-24-hour sleep-wake disorder.
Lifestyle Adjustments and Sleep Hygiene
Lifestyle adjustments and sleep hygiene are important components of a treatment plan for circadian rhythm sleep-wake disorders. This may include avoiding bright light exposure in the evening, establishing a regular sleep schedule, and avoiding stimulants such as caffeine before bedtime.
Counseling and Behavioral Strategies
Counseling and behavioral strategies can also be helpful in managing circadian rhythm sleep-wake disorders. Cognitive behavioral therapy (CBT) can help individuals develop healthy sleep habits and address any underlying psychological factors that may be contributing to the disorder. Additionally, relaxation techniques such as meditation and yoga may also be beneficial.
Overall, treatment for circadian rhythm sleep-wake disorders should be individualized based on the specific needs and circumstances of each individual. A combination of these treatment modalities may be necessary to effectively manage the disorder and improve sleep quality.
Considerations for Specific Populations
Impact on Children and Adolescents
Circadian rhythm sleep-wake disorders (CRSDs) can affect people of all ages, including children and adolescents. In fact, it is estimated that up to 27% of children and adolescents may experience a CRSD at some point in their lives.
One of the most common CRSDs in this population is Delayed Sleep-Wake Phase Disorder (DSWPD), which is characterized by a delayed sleep onset and a delayed wake-up time. This can lead to difficulty falling asleep at a reasonable time, resulting in excessive daytime sleepiness and difficulty waking up in the morning for school or other activities.
Another CRSD that can affect children and adolescents is Advanced Sleep-Wake Phase Disorder (ASWPD), which is characterized by an earlier sleep onset and an earlier wake-up time. This can lead to difficulty staying awake in the evening and difficulty sleeping in on weekends or holidays.
Parents and caregivers of children with CRSDs should work with their healthcare provider to develop a treatment plan that may include behavioral interventions, such as establishing a consistent sleep schedule, avoiding stimulating activities before bedtime, and limiting exposure to electronic devices in the evening.
Circadian Rhythm Changes in the Elderly
As people age, their circadian rhythms may change, leading to disrupted sleep patterns and an increased risk of CRSDs. This is due in part to changes in the body’s production of melatonin, a hormone that helps regulate sleep-wake cycles.
Older adults may also experience changes in their sleep architecture, including a decrease in deep sleep and an increase in lighter, more fragmented sleep. This can lead to increased daytime sleepiness and a decreased ability to concentrate or perform daily activities.
Treatment options for CRSDs in the elderly may include the use of melatonin supplements, light therapy, and behavioral interventions such as establishing a regular sleep-wake schedule and avoiding stimulating activities before bedtime.
CRSDs in Neurodegenerative Diseases
Neurodegenerative diseases such as Alzheimer’s and Parkinson’s can also impact circadian rhythms, leading to disrupted sleep patterns and an increased risk of CRSDs. In fact, up to 90% of people with Alzheimer’s disease experience sleep disturbances.
Treatment options for CRSDs in people with neurodegenerative diseases may include the use of melatonin supplements, light therapy, and behavioral interventions such as establishing a regular sleep-wake schedule and avoiding stimulating activities before bedtime.
It is important for healthcare providers to be aware of the potential impact of neurodegenerative diseases on circadian rhythms and to work with patients and their caregivers to develop a comprehensive treatment plan that addresses both the underlying disease and any associated CRSDs.
Research and Future Directions
Advancements in Circadian Neurobiology
Research in circadian neurobiology has greatly advanced our understanding of the biological mechanisms that regulate the sleep-wake cycle. Recent studies have identified key genes and proteins involved in circadian rhythms, such as CLOCK and PER. Additionally, research has shown that light exposure plays a crucial role in regulating the circadian clock, and that disruptions to this system can lead to sleep-wake disorders.
Emerging Treatments and Technologies
Advancements in technology and medicine have led to the development of new treatments for circadian rhythm sleep-wake disorders. One emerging treatment involves the use of light therapy to reset the circadian clock. This therapy involves exposure to bright light at specific times of day to help regulate the sleep-wake cycle. Other emerging treatments include the use of melatonin supplements and pharmacological agents that target specific proteins involved in circadian rhythms.
Long-Term Studies and Clinical Trials
Long-term studies and clinical trials are essential for evaluating the effectiveness and safety of treatments for circadian rhythm sleep-wake disorders. These studies can help identify potential side effects and determine the optimal dosage and timing of treatments. Additionally, long-term studies can help identify factors that may contribute to the development of sleep-wake disorders, such as genetics, lifestyle, and environmental factors.
Overall, ongoing research in circadian neurobiology, emerging treatments and technologies, and long-term studies and clinical trials are providing new insights into the mechanisms of circadian rhythm sleep-wake disorders and offering new hope for effective treatments.
References:
- Czeisler, C. A., & Gooley, J. J. (2007). Sleep and circadian rhythms in humans. Cold Spring Harbor symposia on quantitative biology, 72, 579-597.
- Wright Jr, K. P., & Czeisler, C. A. (2012). Regulation of sleep and circadian rhythms. Journal of Biological Rhythms, 27(2), 104-114.
- Duffy, J. F., & Czeisler, C. A. (2009). Effect of light on human circadian physiology. Sleep medicine clinics, 4(2), 165-177.
Frequently Asked Questions
What are the treatment options for circadian rhythm sleep-wake disorders?
Treatment options for circadian rhythm sleep-wake disorders vary depending on the specific type of disorder and severity of symptoms. Some common treatment options include behavioral therapy, light therapy, and medication. Behavioral therapy, such as adjusting sleep schedules and creating a consistent sleep routine, can be effective for mild cases. Light therapy, which involves exposure to bright light at specific times of day, can help regulate the body’s internal clock. Medications, such as melatonin or prescription sleep aids, may also be prescribed by a medical professional.
What are common symptoms associated with circadian rhythm sleep-wake disorders?
Common symptoms associated with circadian rhythm sleep-wake disorders include difficulty falling asleep or staying asleep, excessive sleepiness during the day, and difficulty waking up in the morning. Other symptoms may include irritability, difficulty concentrating, and decreased performance at work or school.
Which medical specialists are qualified to treat circadian rhythm sleep-wake disorders?
Medical specialists qualified to treat circadian rhythm sleep-wake disorders include sleep medicine specialists, neurologists, and psychiatrists. Primary care physicians may also be able to diagnose and treat mild cases of circadian rhythm sleep-wake disorders.
How can circadian rhythm sleep-wake disorders impact mental health?
Circadian rhythm sleep-wake disorders can impact mental health by causing symptoms such as irritability, mood swings, and depression. Disrupted sleep patterns can also lead to difficulty concentrating and decreased performance at work or school.
What are the causes behind the disruption of circadian rhythms?
The disruption of circadian rhythms can be caused by a variety of factors, including exposure to artificial light at night, irregular sleep schedules, and certain medical conditions or medications. Jet lag and shift work can also disrupt circadian rhythms.
Are there specific medications effective for managing circadian rhythm sleep-wake disorders?
There are medications that can be effective for managing circadian rhythm sleep-wake disorders, such as melatonin or prescription sleep aids. However, medication should only be prescribed by a medical professional and used as part of a comprehensive treatment plan. Behavioral therapy and light therapy may also be effective for managing circadian rhythm sleep-wake disorders.
Understanding Circadian Rhythm: The Body’s Natural Clock Explained

Circadian rhythms are physical, mental, and behavioral changes that follow a roughly 24-hour cycle, responding primarily to light and darkness in an organism’s environment. These rhythms are driven by an internal biological clock, which is known as the circadian clock or the biological clock.
Continue reading: Understanding Circadian Rhythm
MaryRuth Organics Sleep Gummies Without Melatonin Review: Do They Work?

These gummies are designed to promote relaxation and support sleep quality for adults. Unlike many other sleep aids, they don’t contain melatonin, so you won’t wake up feeling groggy or drowsy.
Continue reading: MaryRuth Organics Sleep Gummies Without Melatonin
Reclaiming Deep Restful Sleep: The Magnesium Deficiency Solution

Discover the natural solution to deep, restful sleep and magnesium deficiency through the efficacy of PUREDOSE® Micelle Liposomal Magnesium. This superior bioavailable supplement promotes optimal sleep support and overall well-being.
Continue reading: Reclaiming Deep Restful Sleep






