Non-24-hour sleep-wake disorder, also known as “free-running disorder,” is a rare sleep disorder that affects a person’s circadian rhythm.
The circadian rhythm is the body’s internal clock that regulates sleep and wake cycles. In people with non-24-hour sleep-wake disorder, their internal clock is not synchronized with the 24-hour day-night cycle, which can lead to irregular sleep patterns and difficulty sleeping at night.
Non-24-hour sleep-wake disorder is more common in blind individuals, particularly those who have been blind since birth. This is because the circadian rhythm is primarily regulated by exposure to light, and without light cues, the body’s internal clock can become desynchronized. However, non-24-hour sleep-wake disorder can also occur in sighted individuals, although it is much less common.
Symptoms of non-24-hour sleep-wake disorder can include difficulty falling asleep at night, excessive daytime sleepiness, and irregular sleep patterns that can shift later and later each day. While there is no cure for non-24-hour sleep-wake disorder, there are treatments that can help regulate sleep and improve quality of life for those affected by this disorder.
Understanding Circadian Rhythms
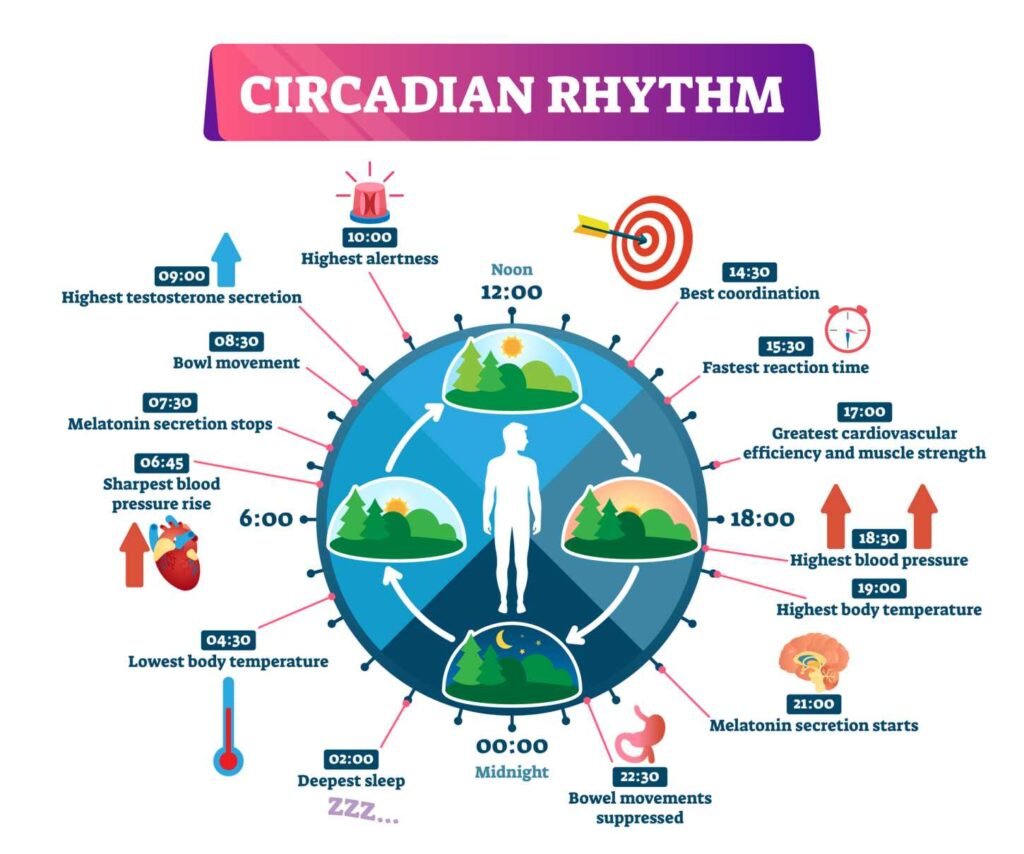
Circadian rhythms refer to the physical, mental, and behavioral changes that follow a 24-hour cycle. These rhythms are regulated by an internal body clock that is located in the suprachiasmatic nucleus (SCN) of the hypothalamus. The SCN is responsible for synchronizing the body’s internal clock with the external environment, including light perception.
The Role of the Suprachiasmatic Nucleus
The SCN receives information about the light and dark cycles from the eyes and uses this information to regulate the body’s circadian rhythms. It sends signals to other parts of the brain and body to adjust hormone levels, body temperature, and other physiological processes. This helps to keep the body in sync with the external environment.
Melatonin and Sleep Regulation
Melatonin is a hormone that is produced by the pineal gland in response to darkness. It helps to regulate the sleep-wake cycle and is an important part of the body’s internal clock. Melatonin levels rise in the evening, helping to promote sleep, and fall in the morning, signaling the body to wake up.
Light exposure can disrupt the body’s production of melatonin, which can affect sleep quality and the body’s internal clock. Exposure to bright light in the evening can suppress melatonin production and make it harder to fall asleep. On the other hand, exposure to bright light in the morning can help to reset the body’s internal clock and improve sleep quality.
In conclusion, understanding the role of circadian rhythms, the suprachiasmatic nucleus, and melatonin can help individuals manage their sleep-wake cycle and improve sleep quality. By paying attention to light exposure and maintaining a regular sleep schedule, individuals can help to keep their internal clock in sync with the external environment.
Non-24-Hour Sleep-Wake Disorder Explained
Characteristics of Non-24
Non-24-hour sleep-wake disorder, also known as Non-24, is a rare circadian rhythm disorder that affects the sleep-wake cycle of an individual. This disorder disrupts the internal body clock, which regulates the sleep-wake cycle. As a result, individuals with Non-24 experience irregular sleep patterns, which can lead to daytime sleepiness, fatigue, and difficulty concentrating.
The symptoms of Non-24 can vary from person to person. Some individuals with Non-24 may experience a gradual shift in their sleep-wake cycle, while others may have a more rapid change. Additionally, some individuals may have a longer sleep-wake cycle than 24 hours, while others may have a shorter cycle.
Prevalence in Blind vs Sighted Individuals
Non-24 is more common in individuals who are totally blind, as they lack the ability to perceive light, which is essential for regulating the internal body clock. Studies have shown that up to 70% of totally blind individuals may have Non-24. However, Non-24 can also affect sighted individuals, although it is much less common.
It is important to note that not all individuals who are blind will develop Non-24, and not all individuals with Non-24 are blind. The prevalence of Non-24 in sighted individuals is not well-established, but it is estimated to be less than 1%.
In conclusion, Non-24 is a rare circadian rhythm disorder that can significantly impact an individual’s sleep-wake cycle. While it is more common in individuals who are totally blind, it can also affect sighted individuals. Understanding the characteristics and prevalence of Non-24 is essential for proper diagnosis and treatment.
Symptoms and Impact on Health
Sleep-Wake Cycle Disruptions
Non-24-hour sleep-wake disorder can cause significant disruptions in the sleep-wake cycle of individuals. The most common symptoms of this disorder are difficulty falling asleep and staying asleep, leading to insomnia. These symptoms are caused by the body’s inability to synchronize with the 24-hour day-night cycle, resulting in an irregular sleep pattern.
Individuals with non-24-hour sleep-wake disorder may also experience excessive daytime sleepiness, which can lead to fatigue and cognitive impairments. They may find it challenging to stay awake during the day and may have trouble concentrating on tasks.
Consequences of Irregular Sleep Patterns
The irregular sleep patterns associated with non-24-hour sleep-wake disorder can have significant consequences on an individual’s overall health. The lack of quality sleep can lead to depression and other mood disorders. It can also weaken the immune system and increase the risk of developing chronic health conditions such as diabetes and hypertension.
In addition, individuals with non-24-hour sleep-wake disorder may find it challenging to maintain a regular work schedule, leading to difficulties in employment and social isolation.
Overall, non-24-hour sleep-wake disorder can have a significant impact on an individual’s quality of life. It is essential to seek medical attention if experiencing symptoms of this disorder to receive proper diagnosis and treatment.
Diagnosis of Non-24
Non-24-hour sleep-wake disorder is a rare circadian rhythm sleep disorder that affects individuals who are totally blind or have no light perception. Diagnosis of non-24 can be challenging due to its rarity and the lack of awareness among healthcare professionals.
Clinical Assessment
Clinical assessment involves taking a detailed medical history and conducting a physical examination to rule out other sleep disorders and medical conditions that may cause similar symptoms. The healthcare professional may also ask the patient to complete a sleep diary to monitor their sleep-wake patterns and assess the severity of symptoms.
Actigraphy and Polysomnography
Actigraphy and polysomnography are objective measures used to diagnose non-24. Actigraphy involves wearing a small device on the wrist that records movement and light exposure. This data is then analyzed to determine the patient’s sleep-wake patterns and circadian rhythm. Polysomnography involves spending a night in a sleep laboratory where various physiological parameters are monitored, including brain waves, eye movements, and muscle activity. This test can help rule out other sleep disorders and identify any underlying medical conditions that may be contributing to the patient’s symptoms.
In conclusion, the diagnosis of non-24 requires a thorough clinical assessment, along with objective measures such as actigraphy and polysomnography. It is important for healthcare professionals to be aware of this rare sleep disorder and consider it as a potential diagnosis in individuals who are totally blind or have no light perception.
Treatment and Management
Medications and Supplements
Currently, there is only one medication approved by the FDA to treat Non-24-Hour Sleep-Wake Disorder (N24SWD), and that is Tasimelteon. Tasimelteon is a melatonin receptor agonist that helps regulate the sleep-wake cycle. However, it is not suitable for everyone, and its effectiveness varies from person to person. Therefore, it is essential to discuss with a doctor before starting Tasimelteon.
Melatonin supplements are also a popular over-the-counter option for managing N24SWD. Melatonin is a hormone that regulates sleep, and taking it in supplement form can help reset the circadian rhythm. However, the effectiveness of melatonin supplements in treating N24SWD is not well-established, and it may not work for everyone.
Non-Pharmacological Interventions
Non-pharmacological interventions can also help manage N24SWD. Light therapy involves exposing oneself to bright light at specific times of the day to help reset the circadian rhythm. Chronotherapy involves gradually adjusting sleep and wake times to align with the desired sleep schedule.
Sleep hygiene and lifestyle changes can also help manage N24SWD. This includes developing a consistent sleep schedule, avoiding caffeine and alcohol close to bedtime, creating a relaxing sleep environment, and engaging in regular exercise.
It is essential to note that there is no one-size-fits-all approach to treating N24SWD. Therefore, it is crucial to work with a doctor to develop an individualized treatment plan that works best for the individual’s specific needs and circumstances.
Living with Non-24
Individuals with Non-24 Hour Sleep-Wake Disorder may face significant challenges in their daily lives due to the unpredictable nature of their sleep-wake cycle. However, there are several adjustments that can be made to help manage the condition and improve overall quality of life.
Daily Life Adjustments
One of the most important adjustments for individuals with Non-24 is to establish a consistent daily routine. This can include setting regular times for waking up, eating meals, and engaging in physical activity. Additionally, it may be helpful to create a relaxing bedtime routine to promote better sleep.
Another important consideration is the use of light therapy. Exposure to bright light in the morning can help reset the body’s internal clock and promote a more regular sleep-wake cycle. Similarly, avoiding bright light in the evening can help signal to the body that it is time to wind down for sleep.
Support and Resources
For individuals with Non-24, it may be helpful to seek support from friends, family, and healthcare professionals. This can include discussing the condition with loved ones to help them better understand the challenges faced by the individual, as well as seeking assistance from healthcare providers to manage symptoms.
In some cases, it may also be appropriate to seek reasonable accommodations under the Americans with Disabilities Act (ADA). This can include adjustments to work schedules or duties to accommodate the individual’s sleep-wake cycle.
Finally, there are several resources available to individuals with Non-24, including support groups and online forums. These can provide a valuable source of information and support for those living with the condition.
Overall, while living with Non-24 can present significant challenges, there are several adjustments and resources available to help manage symptoms and improve quality of life.
Research and Future Directions
Non-24-hour sleep-wake disorder is a relatively rare condition that affects individuals who have difficulty regulating their circadian rhythms. While there is no cure for this disorder, researchers are exploring various treatment options to help individuals manage their symptoms.
Neurology experts are studying the underlying causes of non-24-hour sleep-wake disorder to develop more effective treatments. Recent research has shown that individuals with this disorder have a malfunctioning suprachiasmatic nucleus (SCN), which is responsible for regulating the body’s internal clock. By understanding the mechanisms behind the disorder, researchers hope to develop new therapies that target the SCN and improve sleep-wake cycles.
One promising area of research involves the use of melatonin receptor agonists. These medications can help regulate circadian rhythms and improve sleep quality in individuals with non-24-hour sleep-wake disorder. While more research is needed to determine the long-term efficacy and safety of these medications, they offer a promising avenue for treatment.
As research continues, experts are also exploring non-pharmacological treatments for non-24-hour sleep-wake disorder. Light therapy, for example, has been shown to help regulate circadian rhythms in some individuals. Behavioral therapies, such as cognitive-behavioral therapy for insomnia (CBT-I), may also be effective in managing symptoms.
Overall, while there is still much to learn about non-24-hour sleep-wake disorder, ongoing research is providing new insights into the condition and potential treatment options. As our understanding of the disorder grows, we can hope to develop more effective therapies that improve the lives of individuals with this challenging condition.
Frequently Asked Questions
What are the common symptoms associated with a disrupted circadian rhythm?
Individuals with a disrupted circadian rhythm may experience symptoms such as difficulty falling asleep or staying asleep, excessive daytime sleepiness, fatigue, and irritability. They may also experience changes in appetite, mood, and cognitive function.
How can non-24-hour sleep-wake disorder be diagnosed?
A diagnosis of non-24-hour sleep-wake disorder is typically made based on a combination of medical history, sleep logs, and actigraphy, which is a method of monitoring sleep-wake cycles using a wristwatch-like device. In some cases, a polysomnogram, or sleep study, may also be used to confirm the diagnosis.
What treatments are available for managing non-24-hour sleep-wake disorder?
Treatment for non-24-hour sleep-wake disorder typically involves a combination of behavioral and pharmacological interventions. Behavioral interventions may include maintaining a regular sleep schedule, exposure to bright light in the morning, and avoiding bright light in the evening. Medications such as melatonin and tasimelteon may also be used to help regulate sleep-wake cycles.
What are the underlying causes of non-24-hour sleep-wake disorder?
Non-24-hour sleep-wake disorder is thought to be caused by a disruption in the body’s internal clock, which regulates sleep-wake cycles. This disruption may be due to a variety of factors, including blindness, certain medications, and neurological conditions such as autism and Alzheimer’s disease.
How does non-24-hour sleep-wake disorder affect individuals with autism?
Individuals with autism are at a higher risk for developing non-24-hour sleep-wake disorder due to differences in the way their brains process information. Non-24-hour sleep-wake disorder can further exacerbate the symptoms of autism, including difficulties with social interaction, communication, and repetitive behaviors.
What is the relationship between ADHD and non-24-hour sleep-wake disorder?
There is a high prevalence of sleep disorders, including non-24-hour sleep-wake disorder, in individuals with ADHD. It is thought that the underlying neurobiological mechanisms that contribute to ADHD may also play a role in the development of sleep disturbances. Treating sleep disorders in individuals with ADHD may lead to improvements in ADHD symptoms.
Tasimelteon: A Powerful Treatment for Sleep Disorders

Tasimelteon is a medication that has been approved by the U.S. Food and Drug Administration (FDA) for the treatment of Non-24-Hour Sleep-Wake Disorder in blind individuals.
Continue reading about: Tasimelteon
MaryRuth Organics Sleep Gummies Without Melatonin Review: Do They Work?

These gummies are designed to promote relaxation and support sleep quality for adults. Unlike many other sleep aids, they don’t contain melatonin, so you won’t wake up feeling groggy or drowsy.
Continue reading: MaryRuth Organics Sleep Gummies Without Melatonin