Non-circadian sleep disorders are a group of sleep disorders that affect the timing, quality, and duration of sleep.
These disorders are characterized by the inability to fall asleep or stay asleep at the right time, leading to excessive daytime sleepiness, fatigue, and other health problems. Some of the most common non-circadian sleep disorders include insomnia, sleep apnea, restless leg syndrome, and narcolepsy.
Insomnia is the most common non-circadian sleep disorder, affecting millions of people worldwide. It is characterized by difficulty falling asleep, staying asleep, or both, and can be caused by a variety of factors, including stress, anxiety, depression, and medical conditions.
Sleep apnea, on the other hand, is a disorder in which breathing is interrupted during sleep, leading to snoring, gasping, and other symptoms.
Restless leg syndrome is characterized by an irresistible urge to move the legs, especially at night, while narcolepsy is a neurological disorder that causes excessive daytime sleepiness and sudden sleep attacks.
Non-circadian sleep disorders can have a significant impact on a person’s health and quality of life. They can lead to chronic fatigue, impaired cognitive function, and an increased risk of accidents and injuries.
Treatment options for non-circadian sleep disorders vary depending on the specific disorder and its underlying causes. They may include medications, behavioral therapy, and lifestyle changes such as diet and exercise.
Understanding Non-Circadian Sleep Disorders
Definition and Types
Non-circadian sleep disorders refer to a group of sleep disorders that are not primarily caused by disruptions in the body’s circadian rhythm. These disorders can be caused by a variety of factors, including medical conditions, medications, and lifestyle choices.
There are several types of non-circadian sleep disorders, including sleep apnea, restless leg syndrome, and narcolepsy. These disorders can have a significant impact on a person’s quality of life, and may require medical treatment to manage symptoms.
Circadian Rhythm Basics
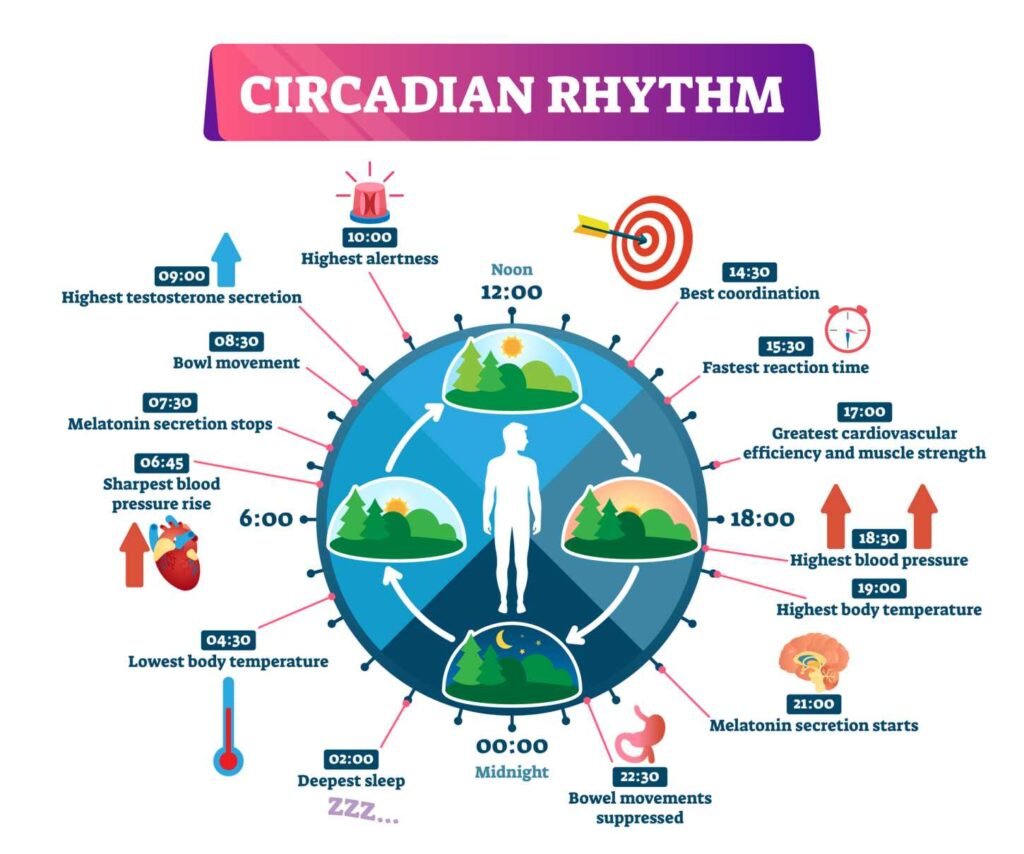
The circadian rhythm is the body’s natural 24-hour cycle of sleep and wakefulness. This cycle is regulated by a part of the brain called the suprachiasmatic nucleus, which responds to environmental cues such as light and darkness.
Disruptions to the circadian rhythm can cause a variety of sleep disorders, including circadian rhythm sleep disorders and non-24-hour sleep-wake disorder. These disorders can cause symptoms such as difficulty falling asleep, waking up too early, and excessive daytime sleepiness.
Role of Melatonin
Melatonin is a hormone that plays a key role in regulating the body’s circadian rhythm. It is produced by the pineal gland in the brain, and is released in response to darkness.
Melatonin supplements are sometimes used to treat sleep disorders such as insomnia and jet lag. However, the long-term effects of using melatonin supplements are not yet fully understood, and it is important to speak with a healthcare provider before using these supplements.
Overall, understanding non-circadian sleep disorders and their underlying causes is an important step in managing these conditions and improving sleep quality. The Circadian Sleep Disorders Network is a valuable resource for individuals seeking information and support related to these disorders.
Non-24-Hour Sleep-Wake Disorder (Non-24)
Characteristics of Non-24
Non-24-Hour Sleep-Wake Disorder (Non-24) is a rare sleep disorder that affects the sleep-wake cycle of an individual. The sleep-wake cycle is a natural process that regulates the body’s sleep and wakefulness. In Non-24, the sleep-wake cycle is disrupted, causing the individual to experience irregular sleep patterns. People with Non-24 may experience periods of insomnia, excessive daytime sleepiness, or both.
Prevalence in Blind and Sighted People
Non-24 is more common in blind people, particularly those who are totally blind, than in sighted people. This is because the sleep-wake cycle is regulated by light exposure, and blind people may not receive enough light exposure to regulate their sleep-wake cycle. However, Non-24 can also affect sighted people, referred to as Sighted Non-24.
Symptoms and Diagnosis
The symptoms of Non-24 can vary from person to person, but typically include irregular sleep patterns, difficulty falling asleep or staying asleep, and excessive daytime sleepiness. To diagnose Non-24, a doctor will typically conduct a sleep study to monitor the individual’s sleep-wake cycle and determine if there is a disruption in their circadian rhythm.
There is currently no cure for Non-24, but there are treatments available to help manage the symptoms. These may include light therapy, melatonin supplements, or prescription medications. It is important for individuals with Non-24 to work closely with their healthcare provider to find the best treatment plan for their specific needs.
In conclusion, Non-24-Hour Sleep-Wake Disorder is a rare sleep disorder that affects the sleep-wake cycle of an individual. It is more common in blind people, but can also affect sighted people. The symptoms of Non-24 can vary, but typically include irregular sleep patterns, difficulty falling asleep or staying asleep, and excessive daytime sleepiness. Diagnosis is typically done through a sleep study, and treatment options include light therapy, melatonin supplements, or prescription medications.
Managing Non-Circadian Disorders
Individuals with non-circadian sleep disorders require a multifaceted approach to manage their symptoms. The following subsections outline various management strategies that can be used to alleviate sleep disturbances.
Light Exposure and Therapy
Light exposure and therapy have been shown to be effective in managing non-circadian sleep disorders. Bright light therapy involves exposure to a light source that simulates natural sunlight, which can help regulate the sleep-wake cycle. This therapy has been shown to be effective in managing symptoms of delayed sleep phase disorder and non-24-hour sleep-wake disorder.
Pharmacological Interventions
Pharmacological interventions may be necessary for individuals with severe symptoms. Tasimelteon, a melatonin receptor agonist, has been approved by the FDA for the treatment of non-24-hour sleep-wake disorder. Melatonin supplements and sleep medication may also be used to manage symptoms.
Lifestyle and Behavioral Adjustments
Lifestyle and behavioral adjustments can also be effective in managing non-circadian sleep disorders. Entrainment, or aligning the sleep-wake cycle with the desired schedule, can be achieved through regular exposure to light and darkness. Phototherapy, or exposure to specific wavelengths of light, may also be helpful. Additionally, practicing good sleep hygiene, avoiding caffeine, and engaging in regular exercise can improve sleep quality and regulate the sleep-wake cycle.
Overall, managing non-circadian sleep disorders requires a comprehensive approach that addresses both the underlying causes and the symptoms. With the right combination of interventions, individuals with non-circadian sleep disorders can achieve better sleep and improved quality of life.
Clinical Considerations and Treatment
Diagnosis and Monitoring
The diagnosis of non-circadian sleep disorders is typically made using the criteria set forth by the American Academy of Sleep Medicine (AASM) in the International Classification of Sleep Disorders (ICSD). The ICSD provides a comprehensive classification of sleep disorders, including non-circadian sleep disorders, and is widely used by sleep specialists and neurologists.
Actigraphy, which involves the use of a wristwatch-like device to monitor sleep and wake activity, is often used to aid in the diagnosis of non-circadian sleep disorders. Additionally, a sleep diary may be used to track sleep patterns and to identify any underlying factors that may be contributing to the disorder.
Polysomnography, a comprehensive sleep study that measures brain waves, heart rate, and other physiological variables, is sometimes used to confirm a diagnosis of non-circadian sleep disorders.
Treatment Options and Effectiveness
The treatment of non-circadian sleep disorders depends on the underlying cause of the disorder. Chronotherapy, which involves gradually shifting the sleep-wake cycle, is often used to treat non-circadian sleep disorders.
Melatonin, a hormone produced by the suprachiasmatic nucleus in the brain, is sometimes used to regulate sleep-wake cycles in non-circadian sleep disorders. Medications such as benzodiazepines and non-benzodiazepine hypnotics may also be prescribed to help regulate sleep patterns.
While treatment options for non-circadian sleep disorders are available, the effectiveness of these treatments can vary depending on the individual and the underlying cause of the disorder.
Challenges in Treatment
One of the challenges in treating non-circadian sleep disorders is identifying the underlying cause of the disorder. Additionally, some individuals may not respond to traditional treatment methods, such as chronotherapy or medication.
It is important for individuals with non-circadian sleep disorders to work closely with their healthcare provider to identify the most effective treatment options for their specific needs. Regular monitoring and adjustment of treatment plans may be necessary to achieve optimal results.
Impact of Non-Circadian Sleep Disorders
Non-circadian sleep disorders can have a significant impact on an individual’s psychological, physical, and social well-being. This section will explore the various consequences of these disorders and their impact on daily life.
Psychological and Emotional Effects
Individuals with non-circadian sleep disorders often experience psychological and emotional effects such as depression, mood swings, stress, and anxiety. They may also have difficulty concentrating and experience memory problems. Chronic sleep deprivation can lead to irritability and a decrease in overall quality of life.
Physical Health Consequences
Non-circadian sleep disorders can also have physical health consequences. Individuals may experience fatigue, excessive daytime sleepiness, headaches, and difficulty falling asleep. The body temperature may also be disrupted, leading to weight gain and other health issues.
Societal and Occupational Implications
Non-circadian sleep disorders can have a significant impact on an individual’s ability to function in society and the workplace. They may require reasonable accommodations to perform their job duties effectively. For sighted individuals, light perception can be a factor in managing their sleep disorder. Travel and shift work can exacerbate the symptoms of non-circadian sleep disorders and make it difficult to maintain a regular sleep schedule.
There may be a genetic component to non-circadian sleep disorders, and certain risk factors such as sex and genetics may increase an individual’s likelihood of developing these disorders. Bipolar disorder may also be associated with non-circadian sleep disorders.
Stimulants and medications may be used to manage the symptoms of non-circadian sleep disorders, but it is important to address the underlying issue and regulate the internal body clock. Overall, non-circadian sleep disorders can have a significant impact on an individual’s quality of life and require proper management to minimize their effects.
Reclaiming Deep Restful Sleep: The Magnesium Deficiency Solution

Discover the natural solution to deep, restful sleep and magnesium deficiency through the efficacy of PUREDOSE® Micelle Liposomal Magnesium. This superior bioavailable supplement promotes optimal sleep support and overall well-being.
Continue reading: Reclaiming Deep Restful Sleep
Discover the Tongue Trick for Better Sleep: The U.S. Marine’s Secret

This tongue trick is designed to help you fall asleep in just two minutes by stimulating a specific nerve in your tongue, known as the “sleep nerve,” to promote relaxation and better sleep.
Continue reading: Discover the Tongue Trick for Better Sleep




