Sleep-related breathing disorders are a group of conditions that affect a person’s ability to breathe properly during sleep.
Sleep-related breathing disorders can range from mild snoring to severe cases of sleep apnea where breathing stops and starts repeatedly throughout the night. Sleep apnea is the most common sleep-related breathing disorder, affecting millions of people worldwide.
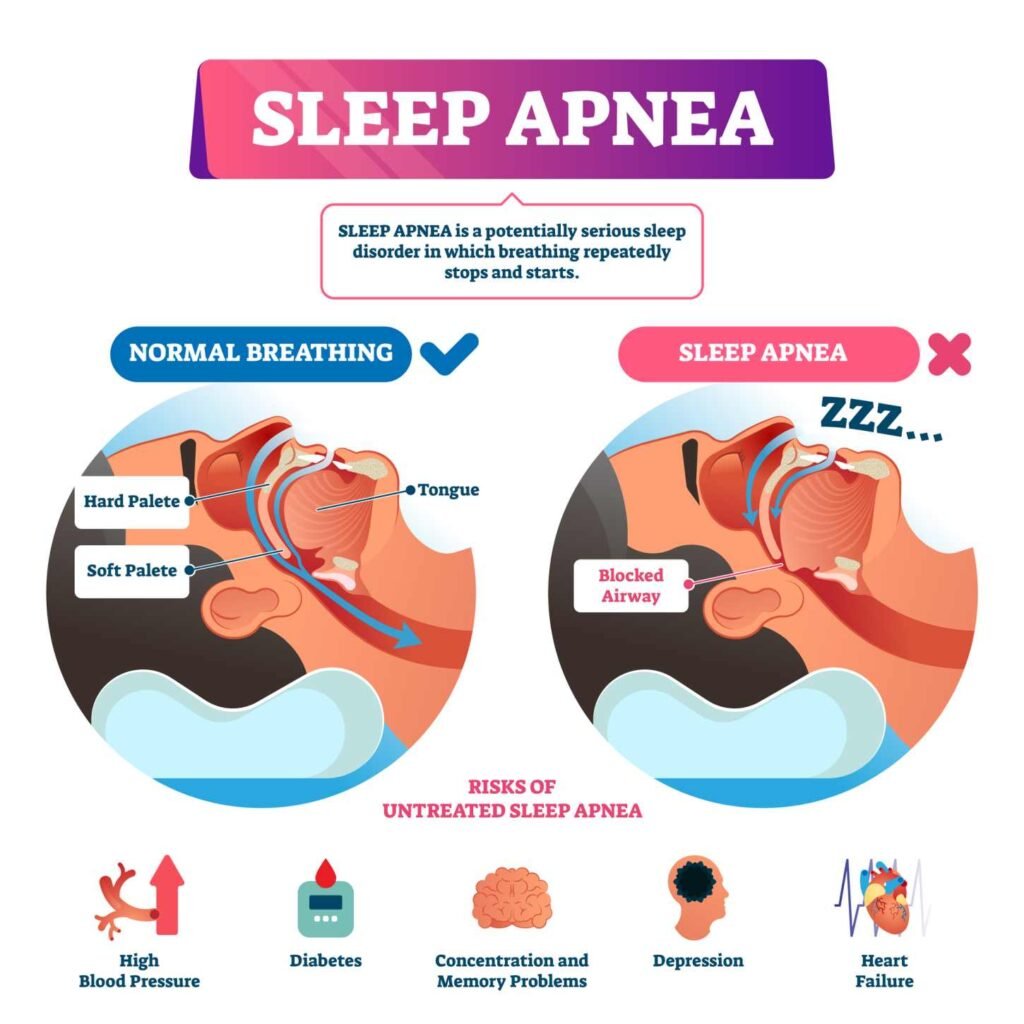
Obstructive sleep apnea is a subtype of sleep apnea that occurs when the airway is partially or completely blocked during sleep. This can lead to loud snoring, gasping or choking during sleep, and excessive daytime sleepiness.
Central sleep apnea, on the other hand, occurs when the brain fails to send the proper signals to the muscles that control breathing. This can result in pauses in breathing during sleep and can lead to a range of health problems if left untreated.
Other sleep-related breathing disorders include upper airway resistance syndrome, hypopnea, hypoventilation, and hypoxemia. These conditions can cause a range of symptoms, including snoring, daytime fatigue, and difficulty concentrating. It is important to seek medical attention if you suspect you may have a sleep-related breathing disorder, as these conditions can have serious health consequences if left untreated.
Understanding Sleep-Related Breathing Disorders
Sleep-related breathing disorders refer to a group of medical conditions that affect the way a person breathes during sleep. These disorders can range from mild snoring to severe breathing disruptions that can lead to serious health problems. Understanding the pathophysiology, classification, and prevalence of these disorders is crucial for their diagnosis and treatment.
Pathophysiology of Breathing Disruptions During Sleep
During sleep, the muscles that control breathing relax, causing the airway to narrow or collapse. This can lead to different types of breathing disruptions, including apnea, hypopnea, hypoventilation, and hypoxemia.
Obstructive sleep apnea syndrome (OSAS) is the most common type of sleep-related breathing disorder. It occurs when the airway is partially or completely blocked during sleep, leading to repeated pauses in breathing. Central sleep apnea (CSA) occurs when the brain fails to send the appropriate signals to the muscles that control breathing. Upper airway resistance syndrome (UARS) is a milder form of OSAS, characterized by increased resistance to breathing without complete airway blockage.
Classification and Types
Sleep-related breathing disorders can be classified based on their underlying causes, symptoms, and severity. The American Academy of Sleep Medicine (AASM) has established a standardized classification system that includes different types of apnea, hypopnea, and other breathing disruptions.
Obstructive sleep apnea syndrome is classified based on the number of breathing pauses or reductions per hour of sleep. Mild OSAS is defined as 5-14 events per hour, moderate OSAS as 15-29 events per hour, and severe OSAS as 30 or more events per hour. Other types of sleep-related breathing disorders, such as CSA and UARS, are classified based on their specific characteristics and symptoms.
Prevalence and Risk Factors
Sleep-related breathing disorders are common, affecting up to 25% of adults in the general population. The prevalence of these disorders increases with age, obesity, and male sex. Other risk factors include smoking, alcohol consumption, nasal congestion, and certain medical conditions.
Obesity hypoventilation syndrome (OHS) is a type of sleep-related breathing disorder that occurs in obese individuals with chronic hypoventilation. It is estimated to affect up to 10% of obese individuals.
In conclusion, sleep-related breathing disorders are a group of medical conditions that can have serious health consequences if left untreated. Understanding their pathophysiology, classification, and prevalence is crucial for their diagnosis and treatment.
Signs and Symptoms
Sleep-related breathing disorders can have a significant impact on an individual’s quality of life. It is important to recognize the signs and symptoms of these disorders to seek appropriate treatment. The following subsections provide an overview of the most common signs and symptoms associated with sleep apnea and related disorders.
Recognizing Sleep Apnea and Related Disorders
Snoring, gasping, and choking during sleep are common signs of sleep apnea. These symptoms occur when the airway becomes partially or completely blocked during sleep, leading to interruptions in breathing. Individuals with sleep apnea may also experience excessive daytime sleepiness, fatigue, morning headaches, and dry mouth upon waking.
Daytime Impacts and Sleep Deprivation
Sleep apnea and related disorders can cause significant daytime impacts, including excessive daytime sleepiness, difficulty concentrating, irritability, and drowsiness. These symptoms can lead to impaired performance at work or school, as well as an increased risk of accidents while driving or operating heavy machinery.
Secondary Health Concerns
Untreated sleep apnea and related disorders can also lead to secondary health concerns. These may include high blood pressure, heart disease, stroke, and diabetes. It is important to seek treatment for sleep-related breathing disorders to prevent these potential health complications.
Overall, recognizing the signs and symptoms of sleep-related breathing disorders is crucial for seeking appropriate treatment and improving quality of life. If you or someone you know is experiencing any of the symptoms listed above, it is important to speak with a healthcare professional for further evaluation and treatment options.
Diagnosis of Sleep-Related Breathing Disorders
Clinical Evaluation by a Sleep Medicine Physician
The diagnosis of sleep-related breathing disorders requires a thorough clinical evaluation by a sleep medicine physician. The physician will take a detailed medical history and perform a physical examination, paying particular attention to the upper airway and respiratory system. The physician will also ask about the patient’s sleep habits, such as snoring, gasping, or pauses in breathing during sleep.
Polysomnography and Other Sleep Studies
Polysomnography (PSG) is the gold standard for diagnosing sleep-related breathing disorders. PSG is a comprehensive sleep study that involves monitoring various physiological parameters during sleep, including brain waves, eye movements, muscle activity, heart rate, and breathing patterns. PSG can also help identify other sleep disorders that may be contributing to the patient’s symptoms.
Other sleep studies that may be used to diagnose sleep-related breathing disorders include home sleep apnea testing (HSAT) and nocturnal oximetry. The home sleep apnea test involves the use of a portable device that the patient wears at home to monitor breathing during sleep. Nocturnal oximetry measures the patient’s oxygen levels during sleep and can help detect episodes of oxygen desaturation that may indicate sleep-related breathing disorders.
Interpreting Diagnostic Indices
The diagnosis of sleep-related breathing disorders is based on the results of polysomnography and other sleep studies. The most commonly used diagnostic indices are the apnea-hypopnea index (AHI) and the respiratory disturbance index (RDI). The apnea-hypopnea index measures the number of apneas and hypopneas per hour of sleep, while the respiratory disturbance index measures the number of respiratory events per hour of sleep, including apneas, hypopneas, and respiratory effort-related arousals.
The American Academy of Sleep Medicine (AASM) has established diagnostic criteria for sleep-related breathing disorders based on these indices. A diagnosis of obstructive sleep apnea is made when the AHI is ≥5 events/hour with symptoms or ≥15 events/hour without symptoms. A diagnosis of central sleep apnea is made when the AHI is <5 events/hour and the RDI is ≥5 events/hour. Mixed sleep apnea is diagnosed when both obstructive and central sleep apnea are present.
Treatment and Management
Lifestyle Modifications and Behavioral Therapy
Lifestyle modifications and behavioral therapy can be effective in managing mild to moderate sleep-related breathing disorders. These modifications involve changes in daily habits and routines that can improve overall sleep quality and reduce the frequency and severity of breathing disruptions during sleep.
Some lifestyle modifications that can be helpful include:
- Weight loss: Losing weight can reduce the amount of fat around the neck and throat, which can contribute to airway obstruction during sleep.
- Positive airway pressure: Positive airway pressure machines, such as continuous positive airway pressure (CPAP) and bilevel positive airway pressure (BiPAP), can help keep the airway open during sleep.
- Oral appliance: An oral appliance can help keep the airway open by repositioning the jaw and tongue.
- Nasal breathing: Breathing through the nose instead of the mouth can help reduce the risk of airway obstruction during sleep.
- Upper airway size: Increasing the size of the upper airway through surgery or other interventions can reduce the risk of airway obstruction during sleep.
Medical Interventions
In some cases, medical interventions may be necessary to manage sleep-related breathing disorders. These interventions can include medication, therapy, and surgery.
Medication may be used to treat underlying conditions that contribute to sleep-related breathing disorders, such as allergies or nasal congestion. Therapy, such as speech therapy or myofunctional therapy, can help strengthen the muscles in the mouth and throat to reduce the risk of airway obstruction during sleep.
Surgery may be recommended in cases where other interventions have been unsuccessful. Surgery can involve the removal of tonsils and adenoids, or the repositioning of the jaw and tongue to increase the size of the upper airway.
Surgical Options
Surgical options for sleep-related breathing disorders may include:
- Uvulopalatopharyngoplasty (UPPP): This surgery involves the removal of excess tissue from the throat, including the uvula, tonsils, and part of the soft palate.
- Maxillomandibular advancement (MMA): This surgery involves moving the upper and lower jaws forward to increase the size of the upper airway.
- Tracheostomy: This surgery involves creating a hole in the neck to bypass the upper airway and allow air to flow directly into the lungs.
Overall, the most effective treatment for sleep-related breathing disorders will depend on the underlying cause and severity of the condition. A combination of lifestyle modifications, medical interventions, and surgical options may be necessary to manage the condition and improve overall sleep quality.
Complications and Comorbidities
Cardiovascular Implications
Sleep-related breathing disorders have been linked to various cardiovascular complications. Hypertension, congestive heart failure, arrhythmias, and other cardiovascular problems have been associated with sleep apnea. Studies have shown that individuals with sleep apnea are at a higher risk of developing hypertension, and that the severity of sleep apnea is positively correlated with blood pressure levels. Furthermore, sleep apnea has been linked to an increased risk of developing congestive heart failure and arrhythmias.
Metabolic and Endocrine Associations
Sleep-related breathing disorders have also been linked to metabolic and endocrine associations. Individuals with sleep apnea are at a higher risk of developing metabolic syndrome, which is characterized by a cluster of metabolic abnormalities such as insulin resistance, dyslipidemia, and obesity. Sleep apnea has also been linked to hypothyroidism and other endocrine disorders.
Mental Health and Cognitive Effects
Sleep-related breathing disorders have been linked to mental health and cognitive effects. Depression, anxiety, and daytime drowsiness are commonly reported in individuals with sleep apnea. In addition, sleep apnea has been linked to cognitive impairment, particularly in the domains of attention, memory, and executive function.
Overall, sleep-related breathing disorders are associated with a range of complications and comorbidities. It is important for individuals with sleep apnea to be aware of these potential health risks and to seek appropriate treatment.
Prevention and Public Health
Awareness and Education
Sleep-related breathing disorders (SRBDs) are a group of disorders that can have serious health implications if left untreated. However, many people with SRBDs are unaware of their condition, and as a result, they may not seek treatment. Therefore, raising awareness about SRBDs is critical in preventing their onset and managing their symptoms.
Public health campaigns that educate people about the risk factors and symptoms of SRBDs can help increase awareness and encourage early detection. In addition, healthcare providers can play a crucial role in educating patients about the importance of getting screened for SRBDs.
Screening and Early Detection
Screening for SRBDs is an essential part of prevention. Early detection of SRBDs can help prevent the development of more severe health problems, such as high blood pressure and heart disease.
Screening for SRBDs can be done in several ways, including a physical examination, sleep study, or home sleep apnea testing. Healthcare providers should encourage patients to get screened for SRBDs if they have any of the risk factors, such as older age, male sex, chronic snoring, chronic nasal congestion, or obesity hypoventilation syndrome.
Policy and Healthcare Implications
Public health policies can play a crucial role in preventing SRBDs. Policies that promote healthy lifestyle habits, such as regular exercise and a healthy diet, can help reduce the risk of obesity, a significant risk factor for SRBDs.
In addition, policies that promote access to affordable and effective healthcare can help ensure that people with SRBDs receive timely and appropriate treatment. Healthcare providers should be trained to recognize the symptoms of SRBDs and provide appropriate treatment to patients.
Overall, prevention and public health efforts can play a significant role in reducing the burden of SRBDs. By increasing awareness, promoting screening and early detection, and implementing effective policies, we can help prevent the development of SRBDs and improve the health outcomes of those affected by these disorders.
Frequently Asked Questions
What are the different types of sleep-related breathing disorders?
There are several types of sleep-related breathing disorders, including obstructive sleep apnea, central sleep apnea, and sleep-related hypoxemia disorder. Obstructive sleep apnea is the most common type and occurs when the muscles in the back of the throat fail to keep the airway open during sleep. Central sleep apnea occurs when the brain fails to send the proper signals to the muscles responsible for breathing. Sleep-related hypoxemia disorder is a condition where the level of oxygen in the blood drops during sleep.
How is obstructive sleep apnea diagnosed and treated?
Obstructive sleep apnea is typically diagnosed through a sleep study, which involves monitoring breathing patterns, heart rate, and other vital signs during sleep. Treatment options may include lifestyle changes, such as weight loss and avoiding alcohol and sedatives, as well as the use of continuous positive airway pressure (CPAP) machines or oral appliances to keep the airway open during sleep.
What are the potential complications of untreated sleep-related breathing disorders?
Untreated sleep-related breathing disorders can lead to a range of health problems, including high blood pressure, heart disease, stroke, and diabetes. They can also cause daytime fatigue, difficulty concentrating, and other issues that can impact quality of life.
What symptoms indicate the presence of a breathing-related sleep disorder?
Common symptoms of sleep-related breathing disorders include loud snoring, gasping or choking during sleep, daytime fatigue, morning headaches, and difficulty concentrating. Other symptoms may include irritability, depression, and decreased libido.
How does central sleep apnea differ from obstructive sleep apnea?
Central sleep apnea occurs when the brain fails to send the proper signals to the muscles responsible for breathing, while obstructive sleep apnea occurs when the muscles in the back of the throat fail to keep the airway open during sleep. Central sleep apnea is less common than obstructive sleep apnea and may be caused by underlying medical conditions or the use of certain medications.
What causes sleep-related hypoxemia disorder and how is it managed?
Sleep-related hypoxemia disorder is caused by a variety of factors, including obesity, smoking, and underlying medical conditions such as chronic obstructive pulmonary disease (COPD) or congestive heart failure. Treatment options may include lifestyle changes, such as weight loss and smoking cessation, as well as supplemental oxygen therapy during sleep.
Understanding Circadian Rhythm: The Body’s Natural Clock Explained

Circadian rhythms are physical, mental, and behavioral changes that follow a roughly 24-hour cycle, responding primarily to light and darkness in an organism’s environment. These rhythms are driven by an internal biological clock, which is known as the circadian clock or the biological clock.
Continue reading: Understanding Circadian Rhythm
MaryRuth Organics Sleep Gummies Without Melatonin Review: Do They Work?

These gummies are designed to promote relaxation and support sleep quality for adults. Unlike many other sleep aids, they don’t contain melatonin, so you won’t wake up feeling groggy or drowsy.
Continue reading: MaryRuth Organics Sleep Gummies Without Melatonin
Reclaiming Deep Restful Sleep: The Magnesium Deficiency Solution

Discover the natural solution to deep, restful sleep and magnesium deficiency through the efficacy of PUREDOSE® Micelle Liposomal Magnesium. This superior bioavailable supplement promotes optimal sleep support and overall well-being.
Continue reading: Reclaiming Deep Restful Sleep





