Sleep-related hypoventilation is a condition that affects a person’s breathing during sleep.
Sleep-related hypoventilation occurs when a person’s breathing rate decreases, causing a buildup of carbon dioxide in the bloodstream. This can lead to symptoms such as fatigue, headaches, and difficulty concentrating during the day.
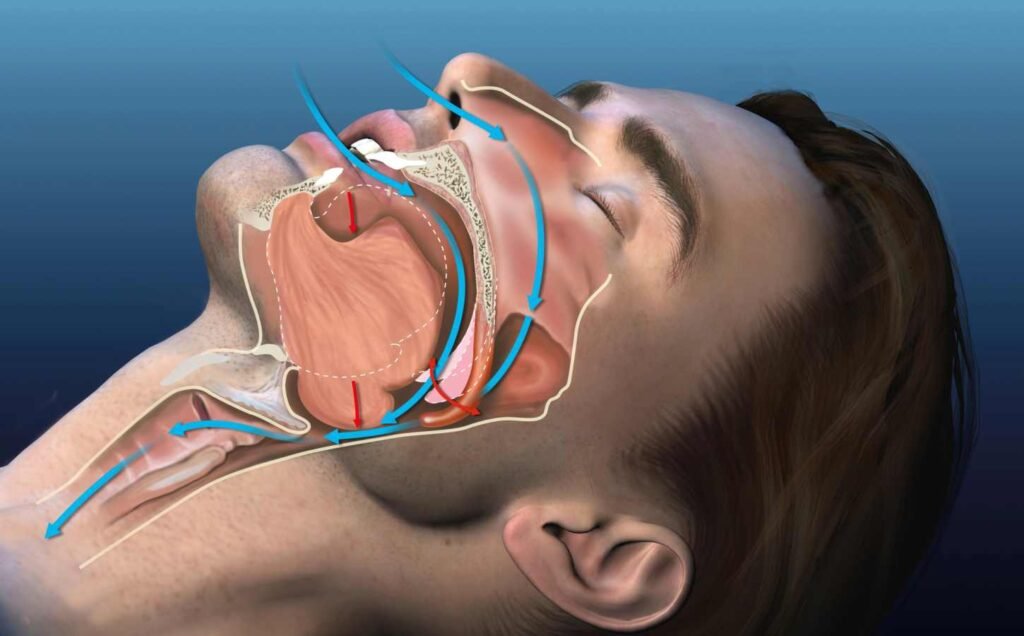
Breathing is a vital function that allows the body to take in oxygen and expel carbon dioxide. During sleep, the body’s breathing rate naturally slows down. However, in people with sleep-related hypoventilation, this slowing down of breathing can become more pronounced, leading to a decrease in oxygen levels and an increase in carbon dioxide levels.
Ventilation, or the movement of air in and out of the lungs, plays a crucial role in maintaining proper oxygen and carbon dioxide levels in the body. When ventilation is compromised, as in sleep-related hypoventilation, it can have significant impacts on a person’s health and well-being. Understanding the causes, symptoms, and treatment options for sleep-related hypoventilation is essential for those who suffer from this condition and their healthcare providers.
Causes and Risk Factors
Sleep-related hypoventilation is a condition that can arise from a variety of underlying causes. Some of the common risk factors and causes of sleep-related hypoventilation are discussed below.
Obesity Hypoventilation Syndrome (OHS)
Obesity is a significant risk factor for sleep-related hypoventilation. When an individual is obese, the excess fat tissue can put pressure on the chest and abdomen, making it difficult to breathe. This can lead to a condition known as obesity hypoventilation syndrome (OHS), which can cause sleep-related hypoventilation. OHS can also lead to other respiratory problems, such as chronic obstructive pulmonary disease (COPD) and pulmonary hypertension.
Neurological and Musculoskeletal Disorders
Neurological and musculoskeletal disorders can cause sleep-related hypoventilation. For example, individuals with neuromuscular diseases such as amyotrophic lateral sclerosis (ALS) or muscular dystrophy may have weakened respiratory muscles, making it difficult to breathe during sleep. Similarly, individuals with spinal cord injuries or chest wall deformities may also have difficulty breathing during sleep.
Chronic Obstructive Pulmonary Disease (COPD) and Other Respiratory Conditions
Chronic obstructive pulmonary disease (COPD) and other respiratory conditions can cause sleep-related hypoventilation. COPD is a group of lung diseases that make it difficult to breathe. Individuals with COPD may experience shortness of breath, coughing, and wheezing, which can worsen during sleep. Other respiratory conditions, such as asthma and pulmonary fibrosis, can also cause sleep-related hypoventilation.
In conclusion, sleep-related hypoventilation can arise from a variety of underlying causes. Obesity, neurological and musculoskeletal disorders, and respiratory conditions are some of the common risk factors and causes of sleep-related hypoventilation. It is important to identify and treat the underlying cause of sleep-related hypoventilation to prevent further complications.
Diagnosis and Treatment
Clinical Assessment and Sleep Studies
Sleep-related hypoventilation is a serious condition that requires prompt diagnosis and treatment. The clinical assessment of this condition involves a thorough evaluation of the patient’s medical history, physical examination, and sleep study. The symptoms of sleep-related hypoventilation may include excessive daytime sleepiness, fatigue, morning headaches, and difficulty concentrating.
Polysomnography is the gold standard for the diagnosis of sleep-related hypoventilation. This test measures various physiological parameters during sleep, including oxygen saturation, carbon dioxide levels, and respiratory effort. The results of this test can help determine the severity of the condition and guide treatment decisions.
Management and Therapeutic Interventions
The management of sleep-related hypoventilation involves treating the underlying cause of the condition, as well as providing respiratory support during sleep. Continuous positive airway pressure (CPAP) is the most commonly used treatment for sleep-related hypoventilation. This therapy involves the use of a mask that delivers a continuous stream of air to keep the airway open during sleep.
Bilevel positive airway pressure (BiPAP) and non-invasive ventilation (NIV) are alternative therapies that may be used in patients who do not respond to CPAP. BiPAP delivers two levels of pressure, one during inhalation and one during exhalation, to help support breathing. NIV uses a machine to deliver air pressure through a mask or nasal prongs to help the patient breathe.
Medications may also be used to treat sleep-related hypoventilation in some cases. These medications may include stimulants to help improve daytime alertness, as well as medications to treat underlying medical conditions that may be contributing to the condition.
In conclusion, sleep-related hypoventilation is a serious condition that requires prompt diagnosis and treatment. Clinical assessment and sleep studies are essential for the accurate diagnosis of this condition. Treatment options include CPAP, BiPAP, NIV, and medications, depending on the severity and underlying cause of the condition.
Sleep-Related Hypoxemia: Causes, Symptoms, and Treatment Options
Sleep-related hypoxemia occurs when the level of oxygen in the blood drops below normal levels, leading to a range of symptoms and potential health risks. This condition is often associated with sleep-related breathing disorders, such as obstructive sleep apnea, and can have serious consequences if left untreated.
Continue reading: Sleep-Related Hypoxemia
Master the 4-7-8 Breathing Technique for Better Sleep
Developed by Dr. Andrew Weil, this technique is designed to promote relaxation and calm the mind, making it easier to drift off to sleep.
The 4-7-8 breathing exercise, also known as the “Relaxing Breath,” is a method that involves a specific pattern of inhaling, holding, and exhaling the breath.
Continue reading: Master the 4-7-8 Breathing Technique for Better Sleep




